Varicose Veins
Varicose veins are the result of vein disease, or venous insufficiency. Veins become dilated, twisting, and bulging, making it difficult to stand, walk, work, or enjoy your favorite activities. Symptoms include itching, heaviness, swelling, and aching in the legs or pelvis. Varicose veins can become a serious medical condition; left untreated, they may cause skin pigment changes, bleeding, skin ulcerations/sores, and blood clots.
Download our illustrated guide to the diagnosis and treatment of varicose veins.
View and Download the Infographic
Understanding Vein Disease
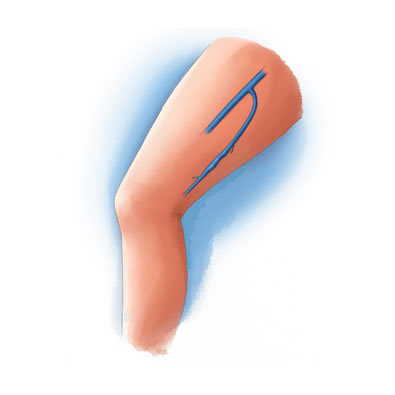
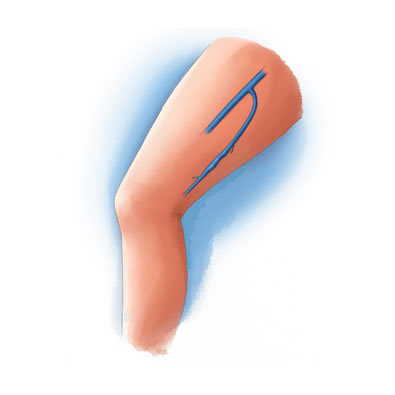
To better understand vein disease (venous insufficiency), you should know the purpose and function of the veins in your body. Healthy veins pump blood back to the heart using one-way valves, which stop blood from moving in the opposite direction. Sometimes these valves weaken, allowing blood to flow backward and pool inside the veins. This backward flow, or reflux, causes a high pressure build-up leading to venous insufficiency.
What is Endovenous Thermal Ablation?
Endovenous thermal ablation is a procedure that uses a laser or high-frequency radio waves to create just the right amount of heat to shrink the problematic veins in the legs. After the vein shrinks, the body automatically routes the blood through other, healthy veins. This procedure is generally performed on large varicose veins.
Endovenous Thermal Ablation Procedure
You will be offered a relaxing medication before the procedure. Your leg is sterilized and local anesthesia is applied to the treatment area.
A catheter is inserted into the vein through a small incision generally below the knee. The ablation device is then inserted into the catheter. When the ablation device is turned on, the heat it generates closes the vein and the catheter is slowly pulled down the length of the vein, closing it permanently.Endovenous thermal ablation is a minimally invasive, in-office procedure that lasts approximately one hour. After the procedure, prescription strength compression stockings must be worn for a short time. However, you’ll be able to resume most normal activities almost immediately. There is virtually no scaring from the procedure because the incision to insert the catheter is only a few millimeters in length.
95% Success Rate
Endovenous thermal ablation is FDA approved and has a success rate of over 95%. As with all surgical procedures, there is a small chance of complication and risks with endovenous thermal ablation.
What is ClariVein®?
ClariVein® Procedure
You will be given a relaxing medication and an anti-inflammatory before the procedure. Your leg is sterilized and prepped for the procedure. The specialized catheter is inserted into the vein through a small incision generally below the knee. Once the catheter is in position inside the target vein, the rotating tip of the catheter is turned on and delivery of the sclerosing agent begins. The catheter is pulled through the length of the vein, closing it permanently. Unlike ablation procedures, this treatment does not use heat, therefore avoiding injections of tumescent anesthesia.
ClariVein® is performed in-office and typically takes an hour. After the procedure, prescription compression stockings must be worn for a short time. You are able to resume most normal daily activities immediately. Currently, insurance coverage for this treatment is limited.
What is VenaSeal™?
VenaSeal™ Procedure
You will be offered a relaxing medication before the procedure. Your leg is sterilized and prepped for the procedure. The treatment catheter is inserted into the vein through a small incision generally below the knee. Once the catheter is in position inside the target vein, small amounts of adhesive are distributed as the catheter is pulled through the length of the vein, closing it permanently. Unlike ablation procedures, this treatment does not use heat, therefore avoiding injections of tumescent anesthesia.
VenaSeal™ is performed in-office and typically takes 1 hour to complete. After the procedure, you are able to resume all activities including strenuous exercise. Currently, insurance coverage for this procedure is limited.

What is Ambulatory Phlebectomy?
Ambulatory phlebectomy removes diseased veins through tiny incisions in the leg. It is primarily used to treat large, painful varicose veins. Because the incisions are small, it leaves undetectable scars. You can generally resume your normal activities the same day.
Ambulatory Phlebectomy Procedure
As an in-office procedure, ambulatory phlebectomy takes 1-2 hours to perform. Before the procedure, an ultrasound and a special light will map the diseased veins. Local anesthesia is injected to the area around veins to be removed. The physician makes several, 2-3 millimeter incisions along the length of the treatment area and using a special hook, removes the diseased veins. After the vein is removed, steri-strips are placed over the incisions. Generally, the incisions do not require stitches.
Following the procedure, a prescription strength compression stocking must be worn for 48 hours night and day and then a majority of the daytime for the next five days. Incisions must also be kept clean and dry for at least five days. With the exceptions of exercise and heavy lifting, you can resume your daily activities immediately.
Over 90% Success Rate
With a long-term success rate of over 90%, ambulatory phlebectomy is an excellent treatment option for veins that can not be treated with standard endovenous thermal ablation techniques.

What is Sclerotherapy?
Sclerotherapy treats varicose veins not visible to the naked eye and veins that make too many twists and turns for standard endovenous ablation procedures. Sclerotherapy is an office-based procedure that involves injecting a sclerosing solution directly into the problem vein. The solution irritates the vein’s wall. Over time, the vein turns into scar tissue, is absorbed back into the body and fades from view.
Sclerotherapy Procedure
Sclerotherapy takes less than an hour to perform. Problem veins are located and mapped using ultrasound or a special light. After the veins have been located, a tiny needle is inserted into the vein and a small amount of sclerosing solution is injected.
Following the procedure a prescription strength compression stocking must be worn for a short time. You can continue most normal activities immediately.
A Highly Successful Procedure
Up to 80 percent of injected varicose veins may be eliminated with each injection session. As with all surgical procedures, there’s a small chance of complication associated with sclerotherapy.

Recovery
Following treatment, you will be able to resume most normal daily activities, although you should refrain from strenuous exercise or heavy lifting for one week. You will also wear a compression stocking for one week post-procedure. Many patients experience mild discomfort, which is typically treated with Ibuprofen or Tylenol. If you choose, ice packs during the first 48 hours after treatment can help with any pain or inflammation. After 48 hours, moist warm compresses will aid the healing process.