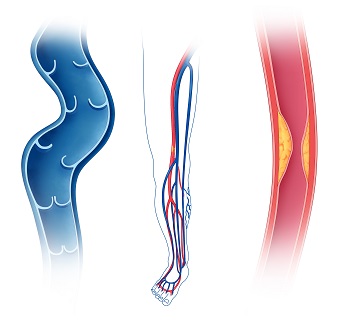
Varicose veins are the result of vein disease, or venous insufficiency. Veins become dilated, twisting, and bulging, making it difficult to stand, walk, work, or enjoy your favorite activities. Symptoms include itching, heaviness, swelling, and aching in the legs or pelvis. Varicose veins can become a serious medical condition; left untreated, they may cause skin pigment changes, bleeding, skin ulcerations/sores, and blood clots.
Learn More
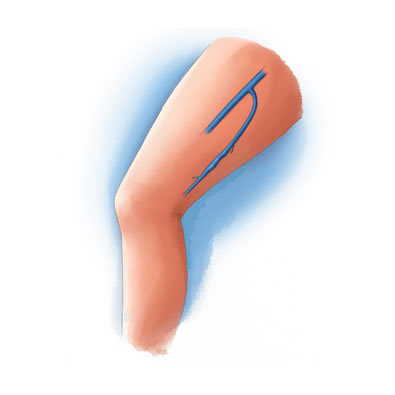
Ambulatory phlebectomy removes diseased veins through tiny incisions in the leg. It is primarily used to treat large, painful varicose veins. Because the incisions are small, it leaves undetectable scars. You can generally resume your normal activities the same day.
Learn More
ClariVein® is a specialty infusion catheter that disperses a sclerosing agent to the target vein, effectively closing it. After the vein shrinks, blood is rerouted to other, healthy veins.
Learn More
Endovenous thermal ablation is a procedure that uses a laser or high-frequency radio waves to create just the right amount of heat to shrink the problematic veins in the legs. After the vein shrinks, the body automatically routes the blood through other, healthy veins. This procedure is generally performed on large varicose veins.
Learn More
Sclerotherapy treats varicose veins not visible to the naked eye and veins that make too many twists and turns for standard endovenous ablation procedures. Sclerotherapy is an office-based procedure that involves injecting a sclerosing solution directly into the problem vein. The solution irritates the vein’s wall. Over time, the vein turns into scar tissue, is absorbed back into the body and fades from view.
Learn More
The VenaSeal™ Closure system uses a proprietary adhesive to close large, problematic varicose veins. Once the vein is closed, blood is automatically routed through healthy veins.
Learn More
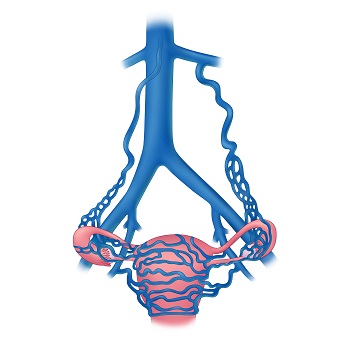
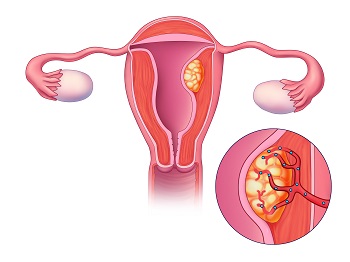
Pelvic congestion syndrome, also called pelvic venous congestion, falls under a broader range of pelvic venous disorders which are a known, but often unrecognized cause of chronic pelvic pain. Varicose pelvic veins develop when the valves in veins are not working correctly, or occasionally when critical deeper veins are obstructed, causing blood to pool and distend pelvic veins.
Learn More
Pelvic venous embolization consists of inserting a thin, flexible, plastic catheter (or tube) into the jugular vein in the neck. Liquid contrast agent is then injected into the veins of the pelvis and special x-rays are obtained. These images allow the doctor to visualize the refluxing pelvic varicosities and seal them off using sclerosant and coils placed inside the abnormal veins.
Learn More
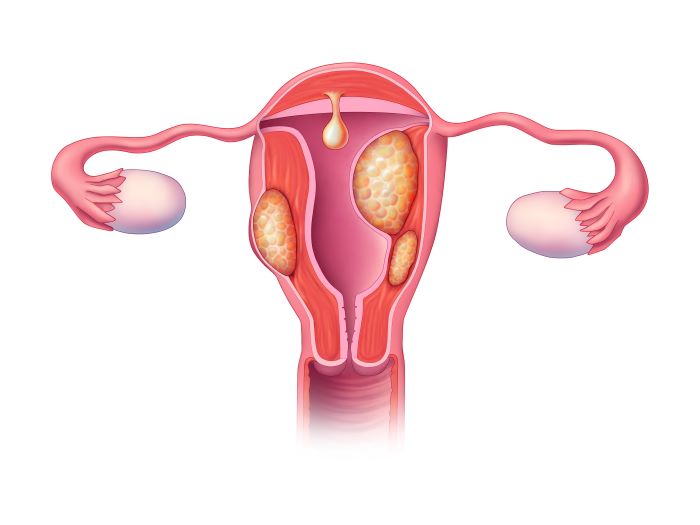
Uterine fibroids are benign tumors that originate from the uterine muscle tissue. Fibroid growth is dependent on estrogen and progesterone and is rare before puberty. Fibroid growth increases in prevalence during the reproductive years and often decreases in size after menopause. Uterine fibroids can cause heavy menstrual bleeding along with a variety of bulk pelvic symptoms.
Learn More
Uterine fibroid embolization, or UFE, targets the abnormal fibroid blood supply which causes the fibroid to shrink. UFE avoids surgery, can preserve your uterus, control symptoms, and improves quality of life. Approximately 9 out of 10 women who undergo uterine fibroid embolization will experience significant symptomatic improvement.
Learn More
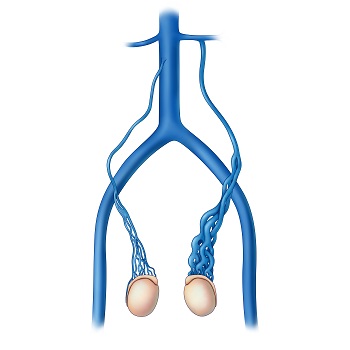
Varicoceles are an important, but often unrecognized cause of chronic groin or scrotal pain. Varicoceles are also associated with infertility. To explain varicoceles, it helps to understand the purpose of veins in the body. Veins help return blood to the heart by preventing backward flow of blood. When valves don’t work or deeper veins are obstructed, blood pools in the congested scrotal veins, resulting in vein distension and increased pressure in the scrotum.
Learn More
Varicocele embolization is performed under ultrasound and x-ray guidance. Your treating physician will guide a small-diameter flexible catheter about the size of a strand of spaghetti into the affected testicular veins. Injection of a liquid contrast agent allows the interventional radiologist to visualize the abnormal refluxing testicular veins and then close these veins using a combination of tiny metal coils and sclerosant.
Learn More
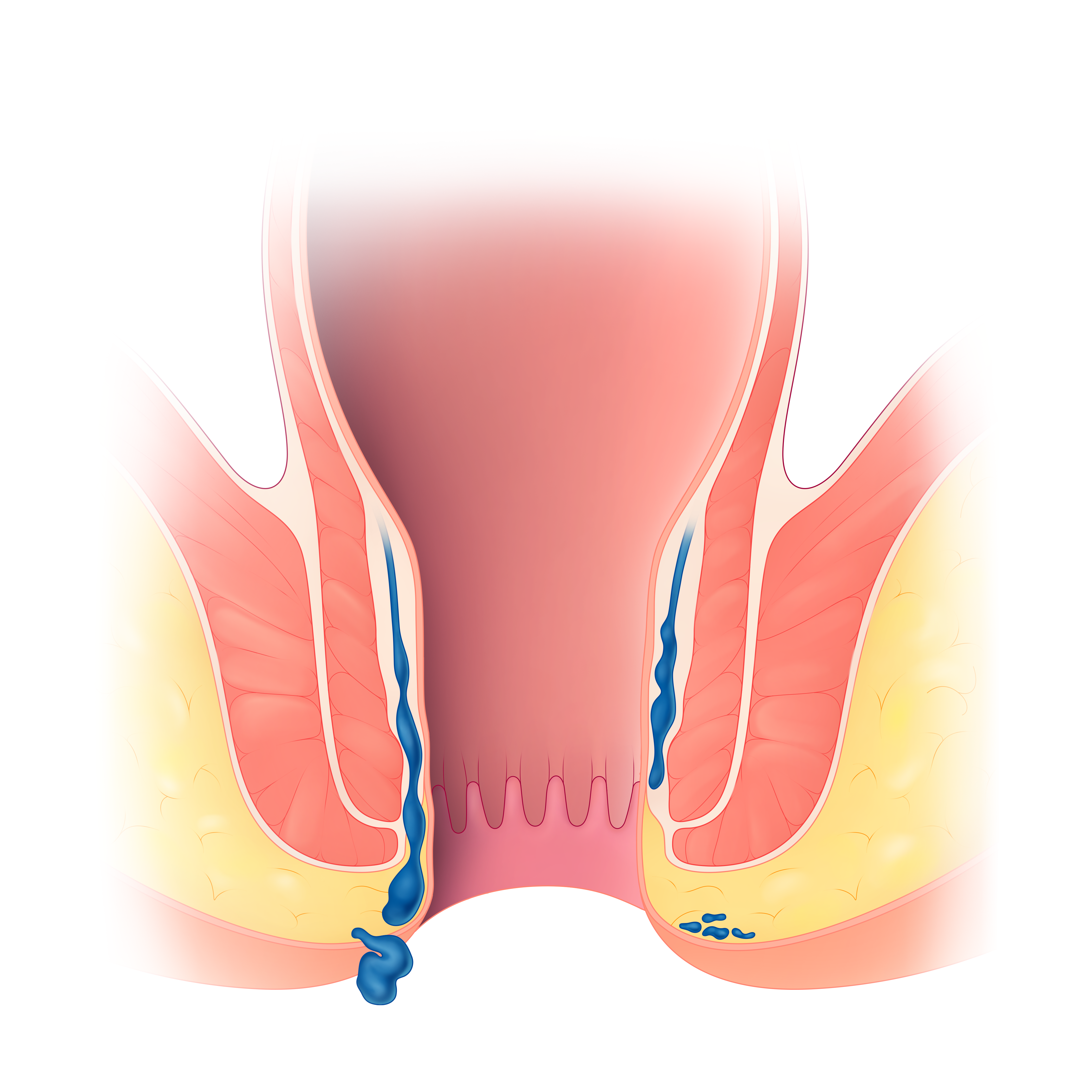
Symptomatic hemorrhoids, also known as piles, are abnormally enlarged and inflamed veins in the rectum and anus caused by increased venous pressure. There are two types of hemorrhoids, internal and external. Internal hemorrhoids occur in the lower rectum while external hemorrhoids are found in the skin around the anus. Symptoms include bleeding, itching, and swelling.
Learn More
Hemorrhoidal artery embolization is a procedure that has been shown to provide long lasting relief from the bleeding, itching, pain and irritation of internal hemorrhoids. HAE is performed in our outpatient lab by our board-certified, fellowship-trained interventional radiologists. The procedure typically takes 45 to 60 minutes.
Learn More
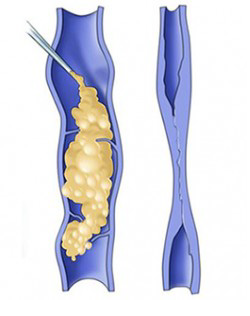
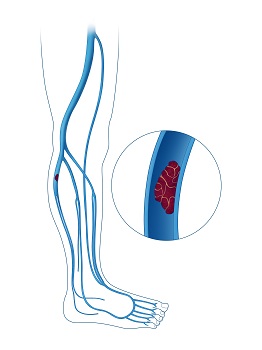
Deep vein thrombosis occurs when a blood clot forms in the deep veins of the body – usually in the leg. While deep vein thrombosis is a fairly common condition, it is also very dangerous. If the clot breaks away and travels through your bloodstream, it could end up in the lungs as a pulmonary embolism – a potentially fatal condition.
Learn More
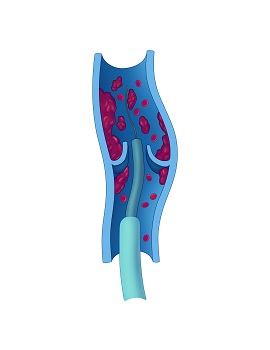
For serious DVT cases that involve larger, more central deep veins, clot can often be removed in order to restore normal flow and prevent scarring and vein occlusion.
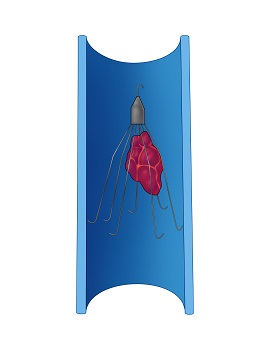
This treatment method is reserved for situations when blood thinners are contraindicated or inefective. The filter prevents large blood clots from passing to the lungs. Filters are typically temporary and are ideally removed when no longer needed.
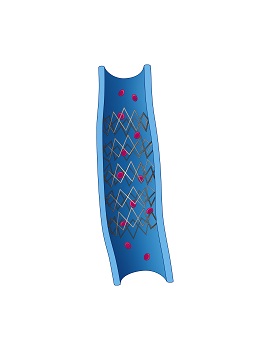
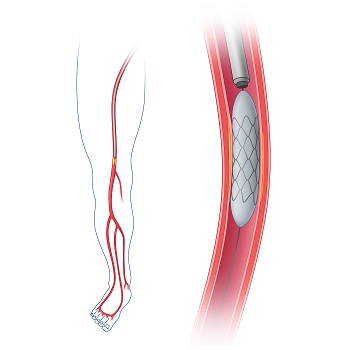
In cases where chronic DVT has resulted in severe symptoms such as leg swelling, skin discoloration and skin ulceration, the larger critical veins may be reopened using angioplasty and stents in order to improve blood flow.
Peripheral arterial disease causes arteries to your arms or legs to narrow or become clogged. This most often results from hardening of your arteries or atherosclerosis. The plaque associated with atherosclerosis blocks blood flow and prevents oxygen from reaching tissue.
Learn More
Angioplasty is a procedure in which a thin, flexible tube called a catheter is inserted through an artery and guided to the place where the artery is narrowed. When the tube reaches the narrowed artery, a small balloon at the end of the tube inflates for a short time. The pressure from the inflated balloon presses the fat and calcium (plaque) against the wall of the artery to improve blood flow.
Learn More
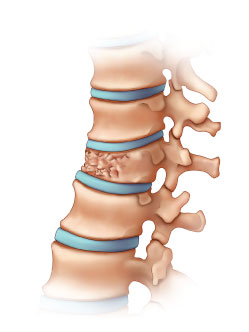
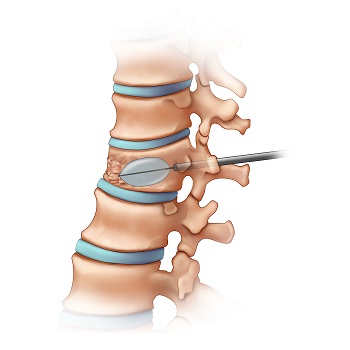
Vertebral compression fractures (VCFs), occur when a vertebral body of the spine collapses. VCFs commonly happen in the mid-to-lower spine and are more common in female and elderly patients.
Learn More
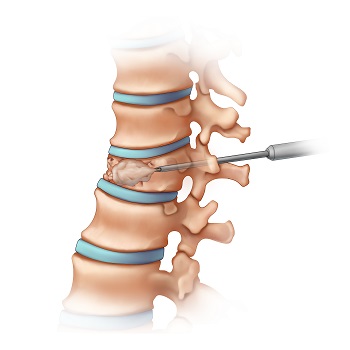
Vertebroplasty involves injecting a quick-setting cement into the fractured vertebra using a small needle. The cement is specially formulated to support broken vertebra and relieve associated pain.
Learn More
The kyphoplasty process is similar to vertebroplasty. Small balloons or mechanical devices are used to elevate the collapsed vertebrae. The doctor then injects quick-setting cement into the vertebral body.
Learn More